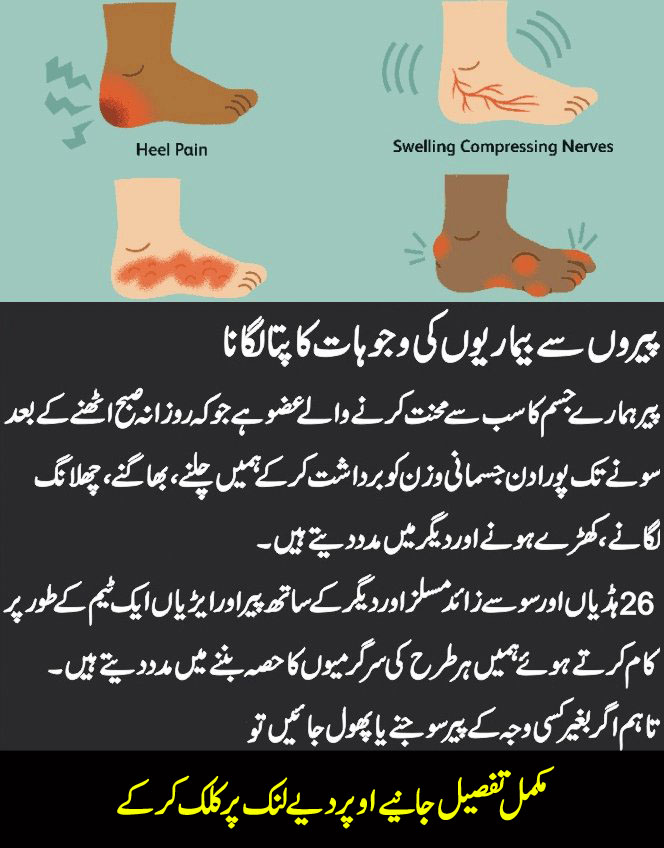
London: My wife is a keen walker but has not been able to walk for months due to heel pain. Her doctor and podiatrist both suggested plantar fasciitis, but it does not hurt in the typical area, and she has not responded to treatment. She is 67. Heel pain, as your wife has found, can be a troublesome and disabling condition. The pain is due to a fat pad contusion, triggered by the breakdown of the protective fat pad underneath the heel, which normally acts as a shock absorber.
The most common causes are plantar fasciitis inflammation of the band of tissue that runs across the bottom of the foot, causing pain around the heel and arch, and Achilles tendon pain, triggered by inflammation of the tendon at the back of the heel.
10 Foot Symptoms And Their Meaning
Things Your Feet Tell You About Your Health
foot
Foot and Nail Care at Home
White Spots On Your Fingernails Mean
fungal infection
Diagnosis of these conditions is usually straightforward, as the pain tends to follow a specific pattern for each. From your longer letter, it sounds as though your wife’s pain is just outside of the typical area for plantar fasciitis.
Investigations, including ultrasound imaging, have confirmed that your wife has a thickening of the Achilles tendon, which suggests there is some inflammation there. You say she has received extracorporeal shockwave therapy, where a device transmits sound waves through the skin of the foot, to increase blood flow to the affected area.
The idea is that this helps reduce inflammation. Studies have shown that this can be effective for plantar fasciitis and Achilles tendinopathy — however, it wasn’t successful for your wife. My suggestion is that the pain is due to a fat pad contusion, triggered by the breakdown of the protective fat pad underneath the heel, which normally acts as a shock absorber.
This can happen as a result of overuse or an injury and may cause persistent pain, especially during long periods of standing or walking. The periosteum (the membrane covering the bone, which contains sensory nerves and blood vessels) may also be less protected, which could be causing your wife’s pain.
This is a less common diagnosis and has no definitive treatment but, in the few cases I have seen it, does ultimately settle. At times, a doughnut-shaped heel pad, available from your chemist, might be of greater value than a full heel pad (you mention your wife wears insoles). Two or three weeks of non-weight-bearing may also help.
This is not an evidence-based suggestion, but it would be worth raising these diagnoses with your wife’s doctor. I am worried about high ferritin levels in my blood — 790 or higher, compared to normal levels of below 400. I have had an ultrasound; what other tests do you recommend to rule out hidden illnesses?
Joe Seet, Sidcup, Kent.
The good news is the tests you detail — an ultrasound of the abdomen and specialized blood tests — would have ruled out any serious diseases.
Ferritin is a protein in the blood that carries iron. A raised level (usually over 400ng/ml in men and 300ng/ml in women) may indicate an overload of iron, but it can also be due to inflammation, for example.
This can be caused by a number of conditions, including metabolic syndrome (a combination of diabetes, high blood pressure, and obesity) and kidney failure, as they cause inflammatory responses. In rare cases, cancer can raise ferritin levels — however, the figures tend to be far higher than yours.
Increased iron absorption may be the result of hereditary hemochromatosis, caused by a faulty gene. In your case, this is a possibility and can be looked into with an additional blood test, the transferrin saturation test. This is available with help from your GP.
Liver disease can also lead to an increase in ferritin, as damage to liver cells will release stored iron into the circulation. If your latest blood tests have excluded liver disease, then it is likely that your raised levels are due to inflammation or infection. This can be confirmed with further blood tests that examine a compound called C-reactive protein (CRP)